MedTruth Q&A with Angie Firmalino
So let’s start with your story, just to contextualize the issues with Essure permanent birth control. I personally believe that we find out who we truly are when we're in the face of adversity. Can you tell me a little bit about your experience and share how it played a role in helping you find your voice?
So, I was implanted in 2009, three months after our son was born. I actually hadn't even heard of Essure and wasn't planning on getting Essure. I had intended during my prenatal visits that if I ended up with a C-section, I wanted my tubes tied.
My first child was a C-section, and though they were 11 years apart, and I was going to try for a vaginal birth, I knew I might end up with a C-section again if I have the same problems. Unfortunately, I had an emergency C section and the on-call physician didn't read my birth plan, didn't talk to me about it, just did the C-section. And I didn't get my tubes tied.
When I went for my post-op with my regular OBGYN, I discussed it with them that
they didn't tie my tubes, but I still wanted to be sterilized. That's when he introduced me to Essure.
He said, “You obviously probably don't want another surgical procedure, you just had a cesarean section. You have a baby and I’m sure you don’t want to have a lot of downtime, so there’s this great new procedure I can do it right in my office can schedule an hour if you want to.”
And I did. So I went and had that done.
So I think I scheduled it like two or three weeks after that appointment. And I went and had it done in the office, not under anesthesia. I didn't have any sedation or medication. I think they gave me a shot of Toradol. They gave me a little bit of Lidocaine, a numbing agent, in my cervix and started the procedure.
It took almost an hour, it was really really painful. He seemed to be struggling, getting them into my tubes and I could feel everything after it was over. I couldn't even get up off the table. It was just so painful, I was cramping, I was having, you know, an anxiety attack just because it was such a prolonged time being under stress and feeling that pain.
So I finally got up and went home and proceeded to just have pain and bleeding for the next several weeks. But when I would call just to touch base and check in, they told me “Well, you know, you're recovering from your C-section, you're recovering from Essure, you just had a baby, you're 37 years old can take your time, your body time to get used to all of these changes. You know, just give it time, give it time, give it time.”
So I kept giving it time and things didn't seem to be getting any better. I started having other problems. I started having fevers and a lot of joint problems. And within about a year of getting Essure, I had my first joint surgery on my left shoulder. Still not making any connections or even thinking about the device.
At this point, my health took a downward spiral. And I really had no idea what was going on.
I finally went in for an annual exam in 2011, and the midwife that was doing the exam asked me how I was doing and what was going on. An I was telling her that I'm bleeding all the time. And she's said, "Define bleeding all the time." I said, “Well, I don't bleed maybe two or three days during the month.” And she just kind of looked at me, she's like, “Whoa, that's, that's not okay. How long has this been going on?” I'm like, “It's been going on for quite some time.”
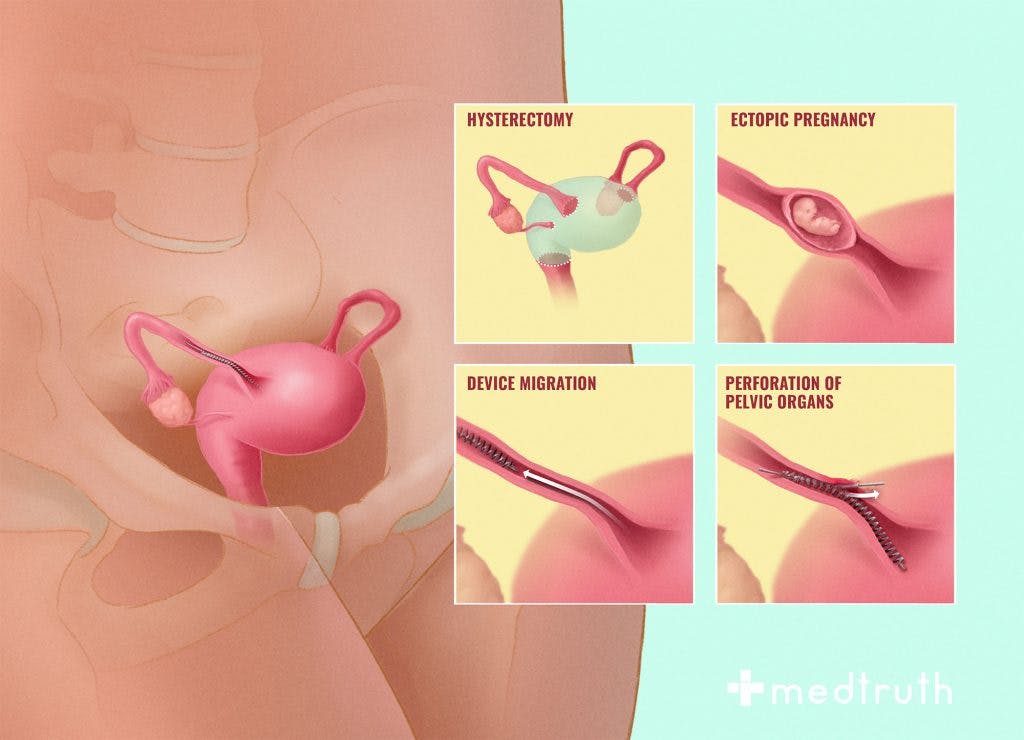
She ordered an ultrasound. And that's when they found out one of my devices was completely embedded in my uterus, and the other one was partially expelling from my fallopian tube.
Sounds like this began with the birth of your child—the failures of the system. From the beginning, not reading your birth plan, not being able to connect the side effects to the Essure device. And I know that after some time you developed a connective tissue disorder, is that correct?
Yeah, that was that was later.
After they had found them in my uterus. And I went through this whole process of interviewing with different physicians, trying to find someone who could take them out. I picked this woman and scheduled removal surgery and she explained how she was going to do it. And it sounded fine at the time.
I didn't know anything about removing these devices, or proper removal or anything. So she said, “We'll put you under general anesthesia. I will go in vaginally and I will cut the embedded coil that's in your uterus. I will cut that one free and take it out. I will look at the other coil and see what position it’s in. If I need to do anything with it, I need to remove it, I will. And then I'll go through your belly button. And I'll do a tubal ligation because obviously, you're not sterile on one side, and possibly not on both sides.”
So I thought that sounded like a great idea. I went through with it came out of surgery. She said everything went fine. She said she took the one out of my uterus that was completely expelled. The other one was mostly expelled, but still a little bit attached to the tube, she cut that one free, took it out, went through the abdomen, did the tubal ligation and I was good to go. So I thought everything was fine. And I went home.
Initially, things felt a little bit better because I had this really intense sharp stabbing pain where the one coil is embedded in my uterus and that was gone. So I felt that go away right away. So it's like, “Okay, I'm on the upswing here.”
But then soon, things started kind of going downhill again.
I started getting really bad headaches. I never had headaches in my life before. I was getting severe, debilitating headaches, the pain started coming back and my lower left side and then the bleeding started picking up again.
So that's when I went online and started researching the removal of Essure and I found one doctor's website that talked about removing them and how they are very fragile. And you can in no way pull on them, cut them, stretch them...they will break and they will fragment.
And then they’ll migrate throughout the body.
Yeah. So I printed that out. I made an appointment to go back to see the surgeon who took mine out. And I went in there with it. And I said, "Listen, I found this online about proper removal. And I'm a little concerned because I'm having these problems again."
And she wouldn't even look at it. I handed it to her. And she handed it right back. She's like, “I got everything out of you. I don't know what your problem is. I don't know what you're concerned about. I’ll order an ultrasound and we'll take from there.” And she walked out of the room.
So I was like a red flag. She ordered an ultrasound. It took a couple of weeks for the office to call me back. They're like, “Well, there's a fibroid, she'll do a D&C.” I said, “What do you mean, there's a fibroid?” she's like, “Well, the doctor says she saw a fibroid. So do you want a D&C?” And I said, “Well, where's the fibroid? Is that where the coil was embedded?” She’s like “What are you talking about?” When I told her she put me on hold for like 20 minutes, came back, and said the doctor will do a D&C.
“Do you want it or not?” I said, "You know what, I don't." And I never went back to her again.
So much disregard for your own safety.
I think she knew that I knew that she did something wrong at that point in that she wasn't being honest with me. Because from that point, I went to my primary care with the printout, he read it and said, “Well, let's do a pelvic X-ray. Let's look.”
We did a pelvic X-ray. And bam, you could see fragments and you know, foreign bodies. And he's like, “You need to order your operative notes from that surgery and you need to order your pathology report. And we need to look and see how she removed these devices.”
So I ordered them they came in the mail, read through the operative notes, which is the surgeons writing out exactly what she did. And she wrote in the operative notes while she was pulling one of the devices out that it broke right there in our own notes. She didn't tell me that and didn't bother to bring it up when I went back to her. She would dismiss me when I went back. I think she knew that I was going to find out.
She had failed and she didn’t want to take responsibility for that. Did she have any prior training to removing the Essure device?
She told me she had removed a few others in the same situation. Of course, none that she had placed, but that other doctors had placed and that expelled, and that she had no problem removing them. And she'd done this before. And that was kind of one of the reasons why I chose her because she was the only one that had said, “Yes, I've seen this before I've done this for other people. I can do this for you." Whereas the other ones who are all male were like, "I don't know what you worried about. Yeah, I can go in there and cut it out. No big deal.”
“What do you what? Why are you complaining? It's no big deal. I'll just go pull it out.”
She was like, “Okay, you know, not a problem. I can take care of this. I've seen it before. I'll make you feel better.” She was just more compassionate about it.
But that doesn't mean that she was more educated.
Exactly. And, you know, at that point, like I said, there wasn't any information. There was no removal protocol on the manufacturers' website. There was nobody talking about removal anywhere else on the internet. Just this one doctor. And it's changed since then, obviously.
That's kind of what spurred me to go, “Hmm, something's not right.”
And then I found that I had fragments. It took me three years after that point to find another OBGYN willing to do a hysterectomy to get the rest of it out of me. No one wanted to touch me.
They're like, “Those little tiny things couldn't possibly...You're too young, you don't want a hysterectomy. I don't really want to mess with anyone else's problems.”
I just kept getting dismissed and dismissed. And finally, one OBGYN who happened to be 75 years old, an old school guy. I went in and I'm like, “Listen, this is what I've been through. I'm, you know, 40, whatever, years old. I'm done having children. I became sterilized because I don't want to have any more children. Actually, I've been sterilized twice. Now I'm bleeding. I'm in pain, I can't have sex. I'm having all these other problems, please. Will you do a hysterectomy?”
And he's like, "Yeah, I will." Thank you. So he did that. But that came with its own problems because at that point, my autoimmune diseases had started kicking in and I wouldn’t heal from things.
So after my hysterectomy, two weeks after all the stitches start dissolving, and my cuff opened up and I hemorrhaged. I had to go in for emergency surgery to repair the vaginal cuff. Two weeks later, the same thing happened had to go into third surgery, another vaginal cuff repair.
So I in and out of the hospital in 2014, I don't even know how many times. I had three surgeries in a row, and then 10 months of silver nitrate. They cauterized the vaginal cuff with this liquid silver nitrate, a chemical burns the cuff, so I had to do that every other week for 10 months. And that was so painful, you know, and then I'd come home from that, and I'd be bleeding and in pain, and I couldn't get out of bed for a couple of days. 2014 was a system nightmare.
You've been through it all, you really have.
Yeah, and then after the first joint surgery, I've had both of my elbows rebuilt. And now, September 13, I have to go in and have surgery on my right shoulder. So, four joint surgeries now.
So you're still in the thick of it, both in your personal life and your advocacy efforts.
TO BE CONTINUED.
The MedTruth Q&A with Angie Firmalino will continue in part two. She'll discuss gender bias in health treatment, failures of federal device regulation, gaps in physician knowledge, and questions about legal compensation. Angie discusses her work with ASHES and provides more information about how people can get involved.